Introduction
The COVID-19 pandemic uprooted lives, taking a decisive toll on children’s health and wellbeing. In 2021, infection in children mimicked that in adults, with rates of hospitalization surpassing many pediatric vaccine preventable diseases (Fleming-Dutra 2022). At the same time, there remained a known risk of serious illness for those with comorbidities or reduced immune protection, and continuation of spread in the community (Kompaniyets et al. 2021; “United States COVID-19 Deaths, Emergency Department (ED) Visits, and Test Positivity by Geographic Area” 2025). However, with the development of the COVID-19 vaccine, pediatricians were given a familiar tool to combat illness and spread of disease.
Although proven to be safe, effective, and available for use in adults since December of 2020, there was pre-emptive hesitancy related to vaccinating children with the new COVID-19 vaccine among families with young children leading up to the approval of the vaccine for use in pediatric populations (Wu, Dudley, Chen, et al. 2021; Zambrano, Newhams, Simeone, et al. 2024). This hesitancy was not only subjectively felt during conversations with families in clinic and hospital settings by pediatric resident providers, but was later found to be true evidenced by reduced vaccine uptake in children. By 2021, in New York State (NYS), 52% of children aged 5-17 years old who were eligible to receive a COVID-19 vaccine had received at least one vaccine compared with >96% for older age groups, with lower uptake among individuals from underrepresented groups (New York State 2022).
Vaccine hesitancy is as old as the advent of vaccine creation, and multifaceted and complex in origin (Betsch et al. 2018; Nuwarda et al. 2022). Broadly speaking, it can be influenced by confidence (trust in vaccine safety), complacency (low perceived risk of acquiring a vaccine preventable disease), constraints (structural and psychological barriers), calculation (engagement in gathering information), and collective responsibility (willingness to protect others). The perceived safety of the COVID-19 vaccine along with the perceived outcomes from a COVID-19 infection have been shown to be the key contributors to COVID-19 vaccine hesitancy—both of which have been amplified by misinformation shared on social media and the Internet (Pourrazavi et al. 2023).
Educating families about vaccination is a vital tool in pediatric care, as a family’s level of scientific knowledge and confidence about vaccine efficacy have both been strongly associated with vaccine uptake overall (“What the American Public Thinks About Vaccines and How Framing Can Help. A Literature Review” 2021). Considering the known benefits of vaccination, including protection from hospitalization and death, it has been and continues to be imperative that pediatric providers combat vaccine hesitancy through improved vaccine education and directly address patient and family concerns with trusted health information (Zambrano, Newhams, Simeone, et al. 2024).
In considering how to most adequately educate families, prior research has shown that visual messaging with identifiable illustrations and relatable graphics can more effectively relay health information, especially for patients with low literacy skills (Rosas-Blum et al. 2018; Houts et al. 2006). Research has also shown that quick response (QR) codes can be effective technological conduits in a variety of healthcare settings to quickly spread essential health information (Basso-Williams et al. 2020; Cho et al. 2021). Separately, collaborations among pediatricians to advocate for the health and social needs of their young patients and families has had a long and successful history, as health advocacy is and has been inextricably tied to the pediatrician’s role. Further, now that advocacy is a core component of pediatric resident training, even more trainees and faculty are engaging in advocacy initiatives and evaluating their impact (Chamberlain et al. 2013; Traba et al. 2021).
Pediatric Residents Take Action
The New York Pediatric Residency Advocacy Coalition (NY PRAC) is a novel trainee initiated and led group of pediatric residents from across institutions in NYS that joined forces to work on advocacy projects. NY PRAC was instituted in fall 2021 by a group of 9 residents from 3 programs across New York City (NYC) who were each advocacy champions at their own health care institutions. This small group of residents wanted to expand their advocacy efforts beyond their own hospitals and clinics, partly based on the recognition that their patients from across the state faced many of the same problems. By joining forces, the residents aimed to reduce redundancy, pool resources, and improve patient care across the city to reach common goals that would have a larger impact than any of them could have alone.
At the first NY PRAC meeting in the fall of 2021, residents expressed that they were seeing a lot of pediatric COVID-19 cases in their clinics and hospital settings, and while the promise of pediatric vaccine approval was coming, vaccine hesitancy was already identified as a perceived barrier. As a result, addressing COVID-19 vaccine hesitancy was the first advocacy project NY PRAC decided to tackle, largely due to its timeliness and potential to impact morbidity and mortality.
To achieve this, this resident-led group of pediatric advocates initiated a formalized collaboration that aimed to produce a pediatric COVID-19 vaccine campaign with the following objectives: (1) work collaboratively with pediatric residents from across NYS to (2) develop visual health literate educational information to address aspects of vaccine hesitancy and disseminate the information throughout their clinic and hospital settings; (3) drive patient families to access trusted health information about COVID-19 vaccines and vaccination; and (4) track the spread of information.
Materials and Methods
NY PRAC held virtual video-conference meetings starting in October of 2021 and continued monthly thereafter to determine the best approaches to develop and disseminate information regarding COVID-19 vaccination. Discussions focused on how to reach the most people through consistent messaging to combat the large amount of misinformation spread on social media platforms. After conducting a literature review on graphical illustrations and technological conduits, it was decided that a poster that caught the eye and included information from trusted sources with strong identifiable scientific backing would have the potential to have the biggest impact. Logistically, the poster would need to be distributed and posted in numerous locations to increase the potential for the same individuals to see it more than once, since the repetition of the same information presented in the same way could provide consistent messaging across pediatric populations. While the group recognized that adults are the ones ultimately making vaccination decisions for youth, the residents decided to keep the focus on youth in their pediatric settings and gear the poster to catch their attention during clinic visits and hospitalizations. The hope was to engage their young patients and then use that connection to spark conversations with their parents and caregivers.
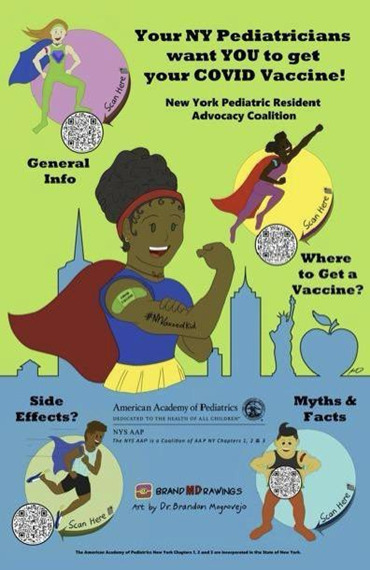
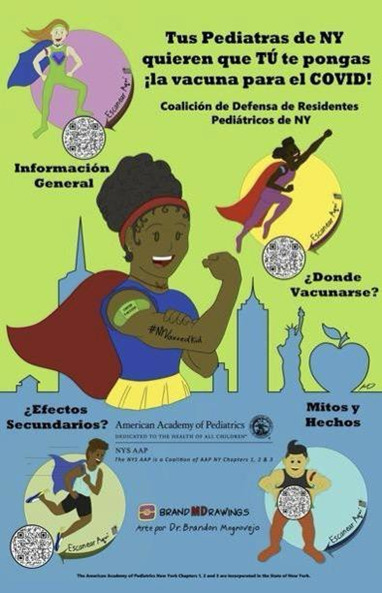
A NY PRAC member volunteered to design and create the poster. Over several video conference meetings, multiple drafts were created to ensure visual representation of relevant patient populations. The Weill Cornell Parental Advisory Group, a group of patients, families, caregivers, hospital staff, and faculty who work together to improve patient and family-centered care, evaluated the poster to provide a community perspective prior to its distribution and confirmed that the poster was family friendly, easy to use, and would be a helpful method to disseminate public health information. The poster was also approved by leadership of the NYS American Academy of Pediatrics (AAP) Chapters 1, 2, and 3, which allowed for the AAP stamp to be included on the poster to give it further credibility. Given the nature of the pandemic, it was decided that there was not enough time to pilot the posters among representative patient populations before distribution.
Quantitative data was collected through QR codes on the final products tracked over time to determine the spread of accessed information. Qualitative and anecdotal feedback was informally shared at NY PRAC meetings about residents’ experiences discussing the posters with their patients.
Results
Goal: Develop and disseminate health literate information to address COVID-19 vaccine hesitancy
The Posters
The final product was a graphic illustration showing multicultural superhero children in the foreground of a NY landscape. Four individual QR codes included on the poster linked to the Centers for Disease Control and Prevention (CDC), which was decided by the group and its advisors to be a politically unbiased and trusted scientific entity. Each individual QR code linked to specific pages that included: general information about COVID-19 vaccines, common myths and facts about the vaccine, side effects to be expected, and a link to sign-up for vaccination appointments. Posters were made available in English (Figure 1) and Spanish (Figure 2).
Image files and detailed instructions about how to print the posters were distributed to NY PRAC members, the AAP Section on Pediatric Trainee NY Delegates, and NYS AAP leadership. NY PRAC meetings and e-mail communications were used to coordinate distribution of posters to all member tertiary care centers. The majority of programs and institutions self-printed the posters in both languages for their own use, while discretionary funds from one institution were used to print posters and distribute them to other programs on request.
Goal: Drive patient families to access trusted health information and track its spread
The Data
Posters were placed in high traffic areas where families could easily encounter them: outpatient waiting and clinic rooms, hospital elevator lobbies, and pediatric floor entrances. Through the first 12 months of distribution, and as NY PRAC itself grew to over 80 members at over 20 residency programs (Figure 3), it was confirmed that the COVID-19 posters were distributed and posted in at least eight centers as reported by NY PRAC members at virtual monthly meetings. However, there was no official count regarding the number posted at each location; this information was not proactively collected or retroactively easy to obtain as not all members attended every NY PRAC meeting due to different residency schedules throughout the year. Nonetheless, since most programs self-printed the posters, more posters were likely displayed than were reported.
During the first year of the NY PRAC COVID-19 vaccination campaign, the QR codes on the posters were scanned 332 times, with distributions by language and section highlighted in Table 1. Unfortunately, it was not possible to link the scans geographically. Anecdotally, NY PRAC members shared their firsthand experiences engaging patients with the posters in their everyday practice. One resident reported engaging an adolescent and their parent in a discussion about vaccination by asking them each to scan one of the QR codes when the resident stepped out of the room, and then to ask one question or convey a concern about what they learned when the resident returned. Another resident reflected on seeing a young child in the hospital elevator tell their parent they wanted to be a superhero like the kid they saw on the poster when they got their own vaccine. Many residents reflected that families would agree to learn one new thing about vaccination before their next visit, even if they were not agreeable to vaccination that day, sparking hope for continued and open conversation down the road.
Goal: Work collaboratively with pediatric residents from across NYS
The Collaboration
The collaboration to develop an educational COVID-19 vaccine campaign was the first project of NY PRAC. In the process, the group learned that individuals passionate about advocacy were able to join together to avoid redundancy and have a larger, more effective voice. Residents reflected that they are often the ones called on to do this kind of educational campaign within their healthcare settings, and this collaborative initiative made it easier and more efficient for them to share ideas and resources to be more effective in their practice.
Resources related to implementing the vaccine campaign were shared amongst and across institutions, such as the printing of posters, to support programs with different levels of funding and capabilities and to ensure that all locations, and therefore the families who seek care there, had equitable access to relevant COVID-19 vaccine information. Practical tips about how to improve the project and address barriers were discussed at monthly NY PRAC meetings. This included shared email templates that were used to gain institutional approval for the posters to be displayed, which underwent multiple iterations based on the success or lack thereof as different members implemented the project, as well as the need to (and how to) laminate the posters before they could physically be displayed in health care facilities based on hospital policies.
Since residents from across programs and locations shared the workload of this advocacy initiative, the challenges often faced when initiating and implementing a timely patient education campaign was lessened in the midst of a highly demanding clinical period during the ongoing COVID-19 pandemic. This was an important aspect of the collaboration because it allowed some residents to be more active during lighter clinical rotations and take a step back as others stepped in when their residencies got busier, without completely halting or significantly delaying this important work and its progress.
Discussion
Overall, the goals of the NY PRAC COVID-19 vaccine campaign, including working collaboratively with residents from across NYS, developing and disseminating health literate information to address vaccine hesitancy, and driving patients and families to access information about COVID-19 vaccines were achieved and can serve as a blueprint for future resident-led advocacy projects of NY PRAC and for others who look to model this work.
Using relatable eye-catching images and simple technology to draw attention and drive individuals to access health literate graphic materials was successful in informing patient families, addressing their questions, and replacing some misinformation about the COVID-19 vaccine. The anecdotal stories from pediatric residents included some unexpected interactions that illustrated the powerful conversations these posters contributed to and that left lasting impressions on both providers and the children and families they care for across NYS and may have led to more vaccinations.
Not all project outcomes were ideal. While >300 scans were recorded across both the English and Spanish posters, it was hoped that this number would have been higher considering the posters were distributed across an entire city and state. Some possible reasons include not displaying as many posters as anticipated, as well as not tracking the number and location of posters distributed and displayed. However, another reason was likely that the posters ended up being used more as conversation starters, which likely did result in fewer codes being scanned, though this was still viewed as a positive outcome primarily because it resulted in building trust with patient families—a key element of patient care and an essential element to address vaccine hesitancy overall.
Another significant limitation of this project was that data was not collected throughout the process. While the lack of data collection was largely tied to prioritizing getting information out to the public over conducting substantive steps prior to implementation to hear from communities directly affected, including through pre- and post-intervention focus groups, residents recognize that these steps have been found to be vital to intervention success. In addition, actual vaccine uptake data was not tracked. Taking these steps would have provided important insights and more concrete data to make improvements going forward for this and future advocacy campaigns. Despite these limitations, this project showed that cross-institutional and cross-program collaboration amongst pediatric residents can be both successful and sustained.
NY PRAC continues to work on a variety of advocacy projects and apply the lessons learned from this vaccine campaign to improve their work going forward. NY PRAC’s current projects include sharing safety information about accidental cannabis ingestion and templates for caring for new immigrants in the healthcare setting. For both projects, the group has met with experts in the NY government to discuss appropriate language and strategies. For these projects, the group is planning for and tracking distribution of information, as well as conducting needs assessments and piloting developed tools prior to implementation to ensure more accurate and robust data collection and that the interventions meet the needs of the groups for which they are designed. NY PRAC will continue to expand and implement new advocacy projects on a bi-annual basis based on current needs identified in the community.
Now in its fourth year, NY PRAC includes even more members representing 20 of the 32 pediatric residency programs in NYS. A structure for permanence was created by enacting multiple co-directors affiliated with different institutions for two-year terms. The leaders tend to be first- or second-year residents, who are then able to transition into mentorship roles during their third year of residency as new residents take the lead. Monthly meetings, minutes, listservs, and shared resource folders ensure all residents who are part of the group are kept informed on current projects and advocacy opportunities. The group communicates via an email listserv and is accessible to the public on Instagram (@nypracoalition) where information is disseminated to both residents and families.
It is the hope of NY PRAC that this vaccine campaign demonstrated to resident physicians the power of their collaboration and the possibilities that can present when like-minded trainees and mentors join together. This formative experience, particularly at such a pivotal life-changing moment for providers and patients during the COVID-19 pandemic, will become even more meaningful as the residents move forward in their practices and future careers to advocate for the overall health and well-being of the children and adolescents in their care.
NY PRAC members encourage pediatric residents from across the U.S. and beyond who seek to create similar collaborations to expand the reach of their advocacy, to connect with them for ideas and support.
Conflict of Interest Disclosures (includes financial disclosures)
The authors have no conflicts of interest to disclose.
Acknowledgments
We thank all members of the New York Pediatric Resident Advocacy Coalition for making this project possible and for their continued dedication to the children and adolescents of New York State. Thank you to the NYS AAP Chapters 1, 2, and 3 for your continued support of NY PRAC and encouragement to make this project possible.
Funding/Support
Support for this project was received from NYS AAP Chapters 1, 2, and 3 for the development and approval of the posters. Poster printing was funded by internal institutions/ Departments of Pediatrics.
Abbreviations:
AAP- American Academy of Pediatrics
CDC- Centers for Disease Control and Prevention
NY- New York
NYC – New York City
NY PRAC - New York Pediatric Resident Advocacy Coalition
NYS- New York State
QR- Quick Response
Author Contributions
MR and DB conceptualized and designed the study, coordinated, and supervised data collection, drafted the initial manuscript, and critically reviewed and revised the manuscript. BM drafted and designed the poster, drafted the initial manuscript, and critically reviewed and revised the manuscript. LG and AS contributed to the design of the study and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.